The Future of Risk Management is Structured Communication

As a risk management professional, we know you are committed to identifying, addressing, and eradicating the root causes of harm that permeate the healthcare industry.
Miscommunication remains the leading cause of medical errors and malpractice cases with communication errors are twice as expensive to defend as those without. Hospitals can no longer afford to ignore the largest crack in the system that consistently leads to medical errors: miscommunication at clinical handoffs. I-PASS partners with organizations across the healthcare ecosystem — from health systems to healthcare liability insurance companies — to deliver a solution that will pay dividends, financially and clinically.
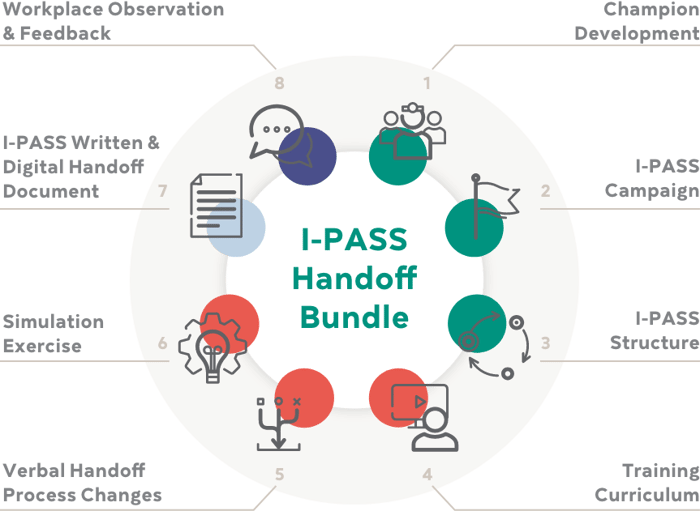
A proven method for seamless care transitions
Developed by clinicians, for clinicians, I-PASS has been the leading authority in structured clinical handoffs for over 15 years. I-PASS handoffs significantly improve safety and quality of care, working directly with healthcare facilities to implement handoff training across the continuum while improving care team communication and culture in the process.
Illness Severity
Stable, “Watcher”, Unstable
Patient Summary
Summary statement; events leading up to admission; hospital course; ongoing assessment; plan
Action List
To-do list; timeline and ownership
Situation Awareness & Contingency Planning
Know what’s going on; plan for what might happen
Patient Summary
Receiver summarizes what was heard; ask questions; restates key action/to do items
Don’t Miss Our Session!
Patient Safety’s Hidden Threat: Variation in Processes and Communication



Christopher Landrigan, MD
Chief, Division of General Pediatrics Boston Children’s Hospital
Dr. Landrigan is Chief of General Pediatrics at BCH, Director of the Sleep & Patient Safety Program at Brigham and Women’s Hospital, the William Berenberg Professor of Pediatrics, and Professor of Medicine at Harvard Medical School. He was a founding member of the Harvard Work Hours, Health & Safety Group, whose work has been a cornerstone in national changes in resident work hours; founding chair of the Pediatric Research in Inpatient Settings Network, the only funded research network for hospitalists in the country, which has attracted more than $50 million in research support and published over 500 peer-reviewed papers; a founder and Principal Investigator of the I-PASS Study Group; a founder of the I-PASS Patient Safety Institute.
Dr. Landrigan has led a series of groundbreaking studies on the epidemiology of medical errors and interventions designed to reduce their incidence. His most important work has been focused on developing reliable patient safety measurement tools and developing and implementing interventions to improve the safety of hospital care. His work on the relationship between resident work hours, sleep and patient safety contributed to national changes in resident work hour standards. Recently he led the development of I-PASS, a multi-faceted handoff & communication improvement program that AHRQ has described as the gold standard for safe handoffs of care; adapting it for use by physicians, nurses and other providers in a wide range of healthcare settings and implementing it. I-PASS has been adopted by pediatric & adult hospitals across the country.
Dr. Landrigan has authored over 200 publications in the medical literature & has received numerous awards for his research, teaching, leadership & innovation. In 2016, the I-PASS Study Group was the recipient of the most prestigious patient safety award in the country, the John M. Eisenberg Award for National Achievement in Patient Safety, from the Joint Commission & the National Quality Forum.


Robert Hanscom
Retired Vice President of Risk Management & Analytics COVERYS
Robert Hanscom, now a strategic advisor for I-PASS Institute, retired from his role as Vice President of Risk Management and Analytics at Coverys in September 2022. During his nine-year tenure at Coverys, he oversaw the company’s national risk management services, and led enterprise-wide initiatives to strengthen Coverys as a data-and-analytics driven organization. Included in those efforts was the development of Coverys’ comparative benchmarking database, which now houses the root-cause factors of approximately 30,000 deeply analyzed malpractice claims. His work has led to a proactive risk management model which focuses on using the evidence to find solutions before harm reaches the patient – rather than after.
Prior to joining Coverys, Robert was with CRICO, the malpractice self-insurance captive for the Harvard system, for 14 years. At CRICO, he was Senior Vice President of Loss Prevention and Patient Safety and headed up CRICO’s external consulting division, CRICO Strategies. Previous to that, Robert was Vice President of Clinical Services at Lahey Clinic in Burlington, MA for a period of five years. Earlier in his career, Robert worked for both Massachusetts General Hospital and for a law practice in Maine. Robert received his B.A. in History from Pacific Union College (California) and his Juris Doctorate from Pepperdine University School of Law.


Pat Folcarelli
Vice President for Patient Safety CRICO
Pat Folcarelli RN, MA, PhD is Vice President for Patient Safety at CRICO the insurance captive for the 35 Harvard affiliated institutions. In her CRICO role Pat assists with strategic and operational patient safety solutions. Pat is a part time lecturer in Medicine at HMS and for the past 4 years has co-directed a course on Patient and Family Engagement in Quality and Safety for the Masters in Healthcare Quality and Safety at Harvard Medical School.
Prior to joining CRICO in 2020, Dr. Folcarelli worked at Beth Israel Deaconess Medical Center (BIDMC) for more than 30 years, most recently as Vice President, Health Care Quality. Pat has worked in health care quality in leadership roles for 22 years.
Pat received her BS in Nursing from Hunter College of the City University of NY and earned both her M.A. and Ph.D. from New York University. She serves on the Quality and Safety Board for Mercy, a health system in St. Louis, MO, and the Board Subcommittee for Quality and Safety Committee of Baystate Health. Pat serves as the Co-Chair of MACRMI (the Massachusetts Alliance for Communication and Resolution Following Medical Injury ) which recently became a part of the Betsy Lehman Center. She has also served on the Board of the Massachusetts Coalition for the Prevention of Medical Errors and is past Board Chair for MITTS (Medically Induced Trauma Support Services) and past President of the Massachusetts Society for Healthcare Risk Management.


Abraham Jacob, MD
Chief Quality Officer M Health Fairview
Abe Jacob, MD, MHA serves as Chief Quality Officer at M Health Fairview, a joint clinical enterprise of a large community health system (Fairview Health Services) and an academic medical center, the University of MN Medical Center/University of MN Masonic Children’s Hospital in Minneapolis, MN. The health system has over 35,000 employees, 10 hospitals, post-acute care and over 70 clinics. After practicing primary care in Internal Medicine/ Pediatrics for 7 years, Abe returned to the University of MN in 2005 to start the first Pediatric Hospitalist program in the Twin Cities area. Abe became Chief Medical Officer at the University of MN Masonic Children’s Hospital from 2012-2018 where he led efforts to reduce preventable harm and implement a high reliability platform focused on patient safety which has now been adopted by the health system. Abe was appointed Chief Quality Officer (CQO) for M Health Fairview in 2019. In his role as CQO, he has oversight over patient and employee safety, regulatory, inpatient and outpatient quality, and infection prevention. He has led efforts to reduce mortality, preventable harm and employee harm across the health system. He continues to practice as an internist and pediatrician in primary care and as a hospitalist at the children’s hospital. He has been married to his partner Christy for over 25 years. Together, they have 7 children, ranging in age from 9-23 years of age.
Structured Communications Are Critical for Proactive Risk Management
49%
of medical malpractice cases include miscommunication
77%
of these cases are preventable with a handoff tool
27%
of all malpractice claim expenses could be reduced with structured communications like I-PASS
Data found in the study “Frequency and Nature of Communication and Handoff Failures in Medical Malpractice Claims,” published in The Journal of Patient Safety, which reviewed a random sample of malpractice claims from 2001 to 2011, collected in CRICO Strategies’ Comparative Benchmarking System.
I-PASS Implementations Lead to Significant Reductions in Costs
Number of Annual Avoidable Events & Costs
| Annual Inpatient Admissions at a 450-bed hospital | 20,000 | |
| Reduction of adverse events per 100 admissions2 | 1.5 | |
| Annual number of adverse events prevented | 300 | |
| Annual Avoidable Costs Range | Cost Per Event | Annual Costs Avoided |
| Low3 | $5,000 | $1.5M |
| Medium4 | $12,000 | $3.6M |
| High4 | $27,000 | $8.1M |
Avoidable Malpractice Claim Costs
| Annual Malpractice Costs | $10.0M |
| % of Malpractice Claims associated with a communication error1 | 49% |
| % of communication errors that include a handoff error1 | 40% |
| % of claims reduced through the use of tools such as I-PASS1 | 77% |
| % of claims potentially avoidable | 15% |
| Relative cost of a handoff related claims to all malpractice claims1 | 179% |
| % of malpractice costs potential avoidable using a tool such as I-PASS | 27% |
| Annual value of malpractice claims potentially avoided | $2.7M |
-
Journal of Patient Safety: March 2022 - Volume 18 - Issue 2 - p 130-137
-
Changes in Medical Errors after Implementation of a Handoff Program. Starmer AJ, Spector ND, et al. N Engl J Med.2014Nov;371:1803-1812, DOI: 10.1056/NEJMsa1405556
-
Costs of adverse events in intensive care units. Kaushal R, Bates DW, Franz C, Soukup JR, Rothschild JM. Crit Care Med.2007Nov;35(11):2479-83.PMID: 1782803
- American Journal of Medical Quality, p1-7, DOI:10.1177/1062860615608938
Resource Hub
CLINICAL STUDY
CRICO/Journal of Patient Safety Study (12 min read)CLINICAL STUDY
Journal of Hospital Medicine Study (10 min read)Our Proud Partners




I-PASS Client Relationships












.png?width=1200&height=1200&name=image%20(1).png)


.png)

FAQS
What do organizations need to have in place for successful I-PASS implementation and sustainment?
We have a detailed organizational readiness assessment to measure a hospital or system’s ability to effectively adopt I-PASS and demonstrate significant impact on patient safety. Following completion of the readiness assessment, the I-PASS Institute will scope the project based on an organization’s internal competencies and bandwidth for successful adoption and sustainment. In many instances, the individual project roles required within an organization for an I-PASS implementation can be internally scoped into the job responsibilities of an existing team member, thus reducing the need for additional resources.
What is the cost and timeline for implementation?
A 300 bed hospital will typically range from $400,000–$500,000 over the three-year implementation period. The cost to maintain the program is significantly reduced post-implementation.
What research or evidence is there to demonstrate the effectiveness of I-PASS?
The I-PASS Study Group is a collaborative of researchers, hospitalists, and medical education specialists who developed a package of interventions to standardize the I-PASS handoff process and study its impact. Once I-PASS was validated, the Study Group became focused on implementing I-PASS in as many hospitals as possible to reduce medical errors and improve patient safety. The Study Group realized that without the appropriate resources, guidance and oversight, hospitals couldn’t implement the program in a way that could be sustained. The I-PASS Institute was created in 2016 to help achieve widespread adoption and sustainment.
Does the I-PASS methodology apply exclusively to handoffs?
The fundamental I-PASS principles can be applied across a variety of care transitions and communication touch points, including handoffs, patient and family rounding, and more.
I’m interested in learning more. How can I get in touch?
To learn more about how the I-PASS program can help your clients, either you or the broker can reach out to our team directly at info@ipassinstitute.com.
Stop by booth #912 to meet our team and learn more about how the I-PASS handoff methodology improves communication and reduces medical errors and malpractice claims.
Request a 30 Min I-PASS Explainer
Connect with Marshall to discuss how I-PASS Training can help healthcare facilities significantly reduce adverse events, keep patients safe, and minimize the financial burden of medical malpractice.
Reach out to us directly with questions or connect us with your clients directly by sending us an email at info@ipassinstitute.com.
Stop by booth #912 to meet our team and learn more about how the I-PASS handoff methodology improves communication and reduces medical errors and malpractice claims.
Request a 30 Min I-PASS Explainer
Connect with Marshall to discuss how I-PASS Training can help healthcare facilities significantly reduce adverse events, keep patients safe, and minimize the financial burden of medical malpractice.
Reach out to us directly with questions or connect us with your clients directly by sending us an email at info@ipassinstitute.com.
Read More About Improving Clinical Handoffs
At I-PASS, we’ve been researching, studying, and solving for miscommunication in clinical settings since 2008. We’ve positively impacted millions of handoffs, literally, and are passionate about improving care by any means possible. We’ve pleased to share all of our available resources with you — and if you don’t see what you’re looking for, reach out.
Useful Links
Evidence
Get in Touch
Boston, MA 02108

